Heart and Mind: New Studies Unravel Link Between Cardiovascular Disease and Dementia
Bridging the Knowledge Gap Between Neurology and Cardiology Could Foster a More Integrated Approach to Patient Care
Cardiovascular disease and dementia are two significant and devastating health challenges that are becoming more prevalent as global populations age—an estimated 50 million people worldwide are living with dementia, a figure expected to triple by 2050. With growing evidence highlighting the strong interconnection between cardiovascular disease and dementia, bridging the knowledge gap between neurology and cardiology is even more critical to fostering a more integrated approach to patient care. Two recent studies by New York Medical College students and faculty, published in Cardiology in Review, shed light on this crucial connection.
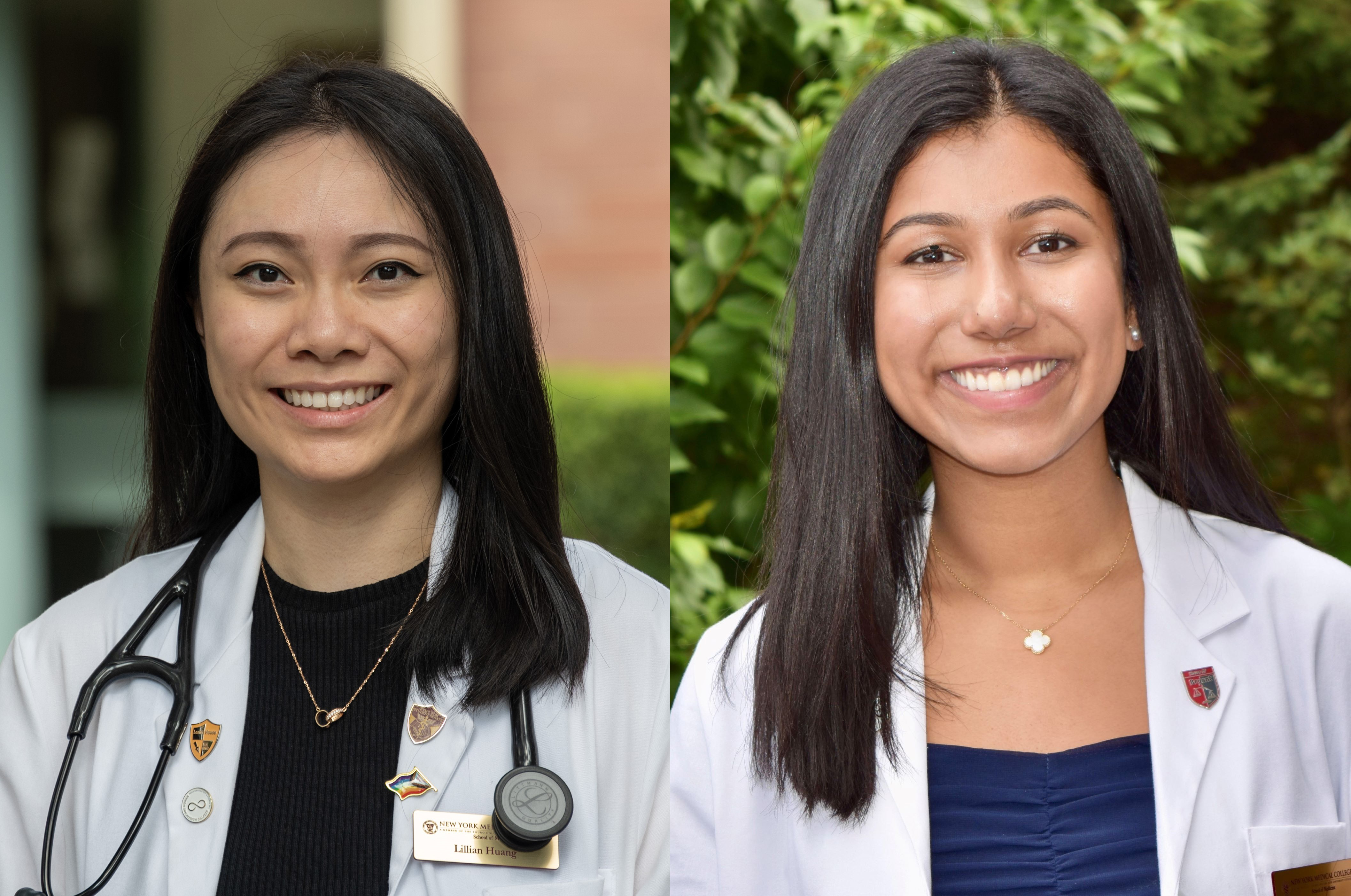
“While atherosclerosis is widely recognized for its role in coronary artery disease (CAD), its impact on brain health and the progression of dementia has not been as deeply explored,” says Anjali Goyal, SOM Class of 2026, who was lead author on a study focused on the connection between dementia and myocardial infarction. “By studying both conditions together, we can better understand how vascular health impacts multiple organs and systems, potentially leading to more holistic approaches in managing patients at risk for both CAD and dementia.”
“Hypertension is emerging as a variable risk factor for major neurocognitive disorders, contributing to neurodegenerative processes through vascular damage, inflammation, and blood-brain barrier disruption. However, the role of antihypertensive treatments in preventing or treating cognitive decline remains unclear, with mixed evidence varying by antihypertensive class and the type of neurocognitive disorder,” says Lillian Huang, SOM Class of 2026, who was lead author on a study exploring the therapeutic challenges regarding cardiovascular disease and dementia.
The hope is that findings from both studies could lead to a more nuanced approach to prevention and treatment—highlighting potential avenues for early intervention and risk reduction for dementia and Alzheimer's disease.
“Clinicians might consider hypertension not only as a cardiovascular risk factor but also as a potential contributor to cognitive health, adjusting treatment goals accordingly,” says Huang. “For patients with a family history or other risk factors for major neurocognitive disorders, selecting antihypertensive medications such as angiotensin-converting enzyme inhibitors or calcium channel blockers could offer dual benefits in cardiovascular and cognitive health.”
“Given the shared role of atherosclerosis in both CAD and dementia, clinicians may need to consider cardiovascular risk factors more carefully when assessing dementia risk, and vice versa. Interventions already used to manage heart disease, such as statins, lifestyle changes, or other therapies that improve vascular health, might also prove useful in slowing the progression of cognitive decline in at-risk populations,” says Goyal.
For Goyal, one of the key questions that remains unanswered is whether aggressive treatment of atherosclerosis can directly reduce the incidence of dementia. “While we know there is a connection, it's still unclear whether targeting atherosclerotic plaques early on will definitively slow cognitive decline. Moving forward, we plan to explore whether specific interventions aimed at improving vascular health could have a more direct impact on reducing the risk of dementia.”
Also key to combating dementia and cardiovascular disease is improved patient education on managing risk factors, such as diabetes, smoking, and weight, and making healthy choices. “Heart-healthy choices—such as regular exercise, quitting smoking and heavy drinking, and a balanced diet—may not only protect you from heart disease but also reduce your risk of dementia later in life,” says Goyal. “Small, consistent steps toward maintaining good vascular health can have long-lasting benefits.”

