The School of Medicine (SOM)’s undergraduate medical degree program offers comprehensive medical training in an inspiring, supportive atmosphere. The integrated M.D. Program curriculum provides you with a strong foundation in biomedical sciences and robust, longitudinal clinical skills training. Early clinical exposure ensures that you gain both theoretical knowledge and practical skills and can respond and relate to patients with equal parts competence and compassion.
If you are looking to become a highly capable clinician with the skills that inspire trust and confidence in your patients, our program is for you.
The foundational knowledge, clinical experience and specialized skills you learn in our program will prepare you for your residency and a fulfilling, lifelong career in medicine.
M.D. Curriculum
The curriculum in the M.D. program prepares physicians to practice medicine skillfully and compassionately. You’ll be ready to practice in a diverse world where technological advances and evolving regulatory issues present continual challenges and opportunities. Our curriculum is designed so you can meet specific competency requirements as a physician upon graduating.
Our integrated curriculum promotes critical thinking and self-directed learning and reflects contemporary issues facing physicians today. We train exceptional, self-directed, compassionate physician leaders dedicated to the health and well-being of all patients and populations.
Relevant curricular themes are interwoven throughout the M.D. Program to create opportunities for progressive foundational learning. Examples of prioritized thematic curricula include Health Systems Science, Racism and Bias in Medicine, Medical Imaging, Nutrition, Genetics and Women's Health.
The Three Phases of Medical School
The M.D. Program curriculum is divided into three phases: Foundational Sciences, Core Clerkships, and Advanced Practice. The following sections give an overall summary of your medical school curriculum.
Phase One / Foundational Science Phase
Phase One of the M.D. Program is organized into six courses, each of which integrate foundational, clinical and health systems sciences. Phase One lasts 18 months and incorporates a variety of instructional modalities including large group and small group interactive exercises, laboratories, self-directed learning, standardized patient encounters and medical simulation. There is an additional course, The History of Medicine, delivered in the spring of the M1 year, which allows you to examine the interplay of gender, culture, religion and science over time.
Students take the United States Medical Licensing Examination® (USMLE) Step 1 after completing Phase One of the M.D. Program.
Hands-On Patient Care Experiences
Complementing your classroom learning during Phase One community-based service learning and a longitudinal clinical preceptorship program are required. Beginning during the first week of medical school, you learn and practice basic interviewing, communication skills and physical examination techniques in NYMC’s Clinical Skills and Simulation Center, as well as work directly with actual patients in community service learning programs and clinical settings with faculty providing direct mentorship. Through these hands-on experiences, you’ll learn “on the job” and put theory into practice.
Phase 1, Year 1:
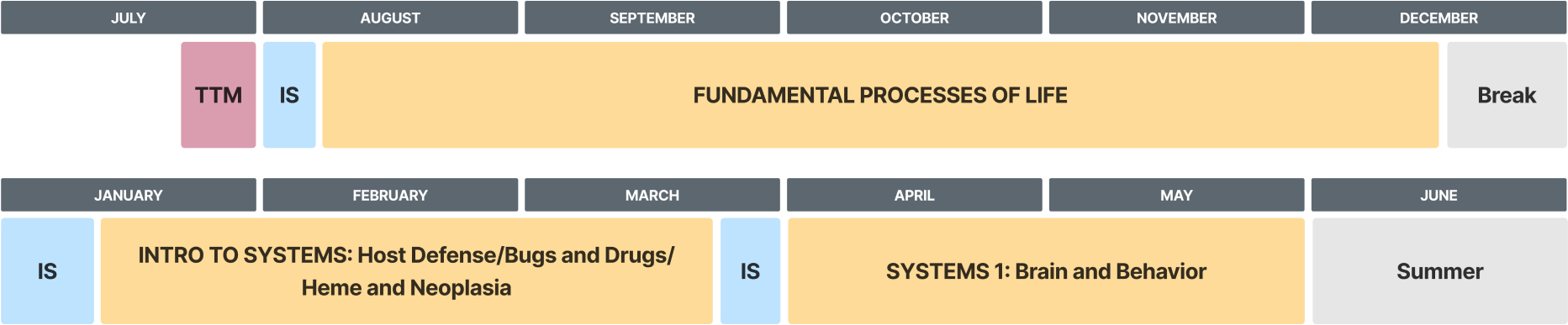
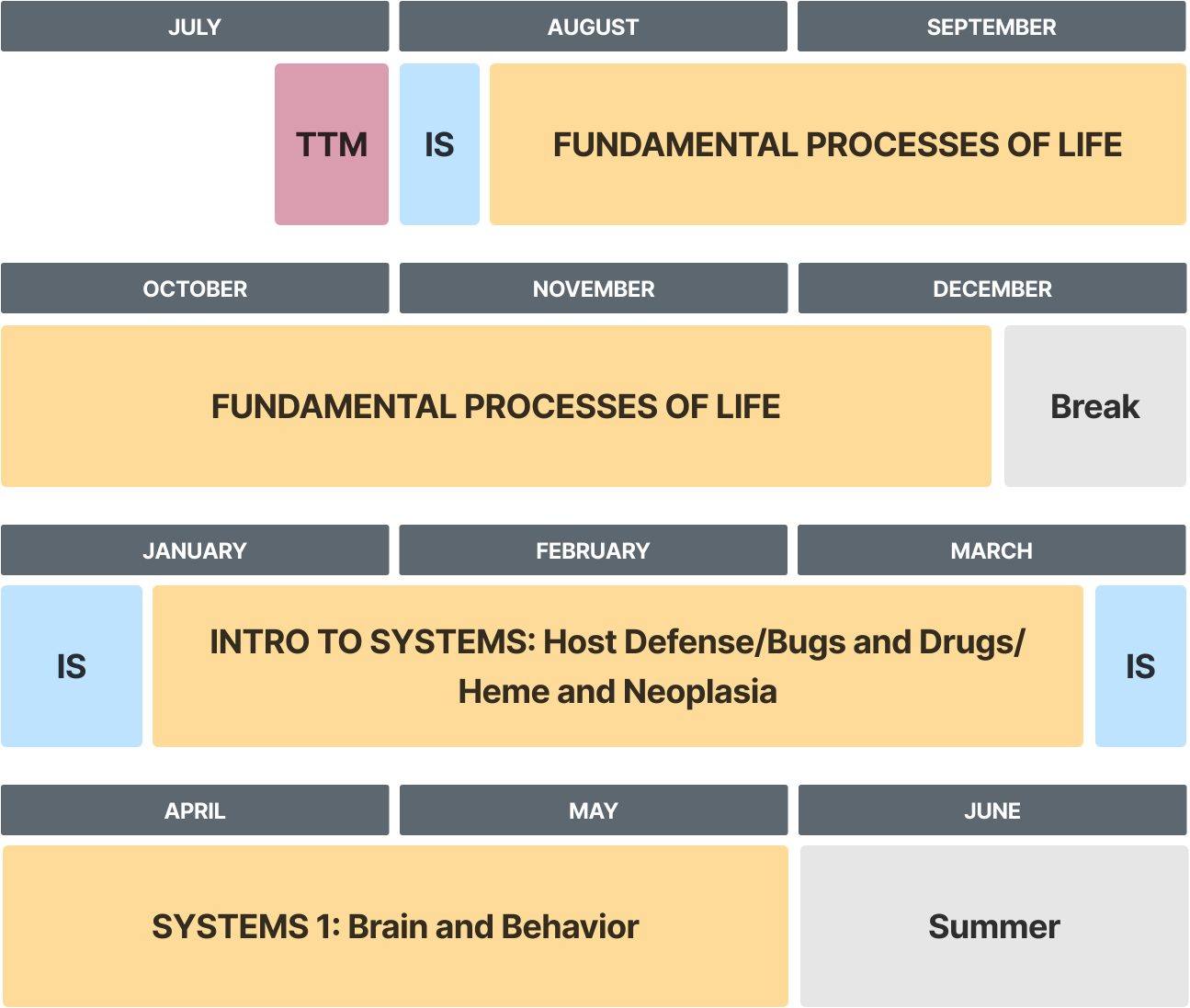
KEY- TTM: Transition to Medical School, IS1-5: Health System Science Intersessions. This is a sample schedule. Individual student schedules may differ. Curriculum subject to change.
Chart Description
A sample schedule of phase 1 of year 1 of the M.D. program. It starts with "Transition to Medical School (TTM)" at the end of July, followed by "Health System Science Intersession (IS)" at the beginning of August. "Fundamental Processes of Life" runs from August through mid-December, followed by a break for the remainder of December. In January, another "IS" session begins, followed by "Introduction to Systems," covering topics like Host Defense, Bugs and Drugs, Heme, and Neoplasia from January to March. Another "IS" session occurs at the end of March. "Systems 1: Brain and Behavior" is covered from April to May, leading into the summer break in June.
Phase 1, Year 2:
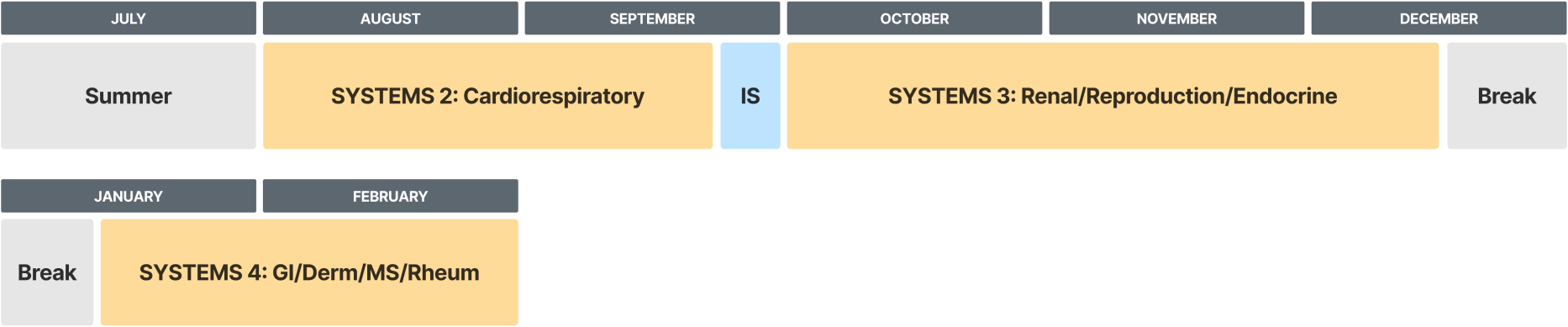
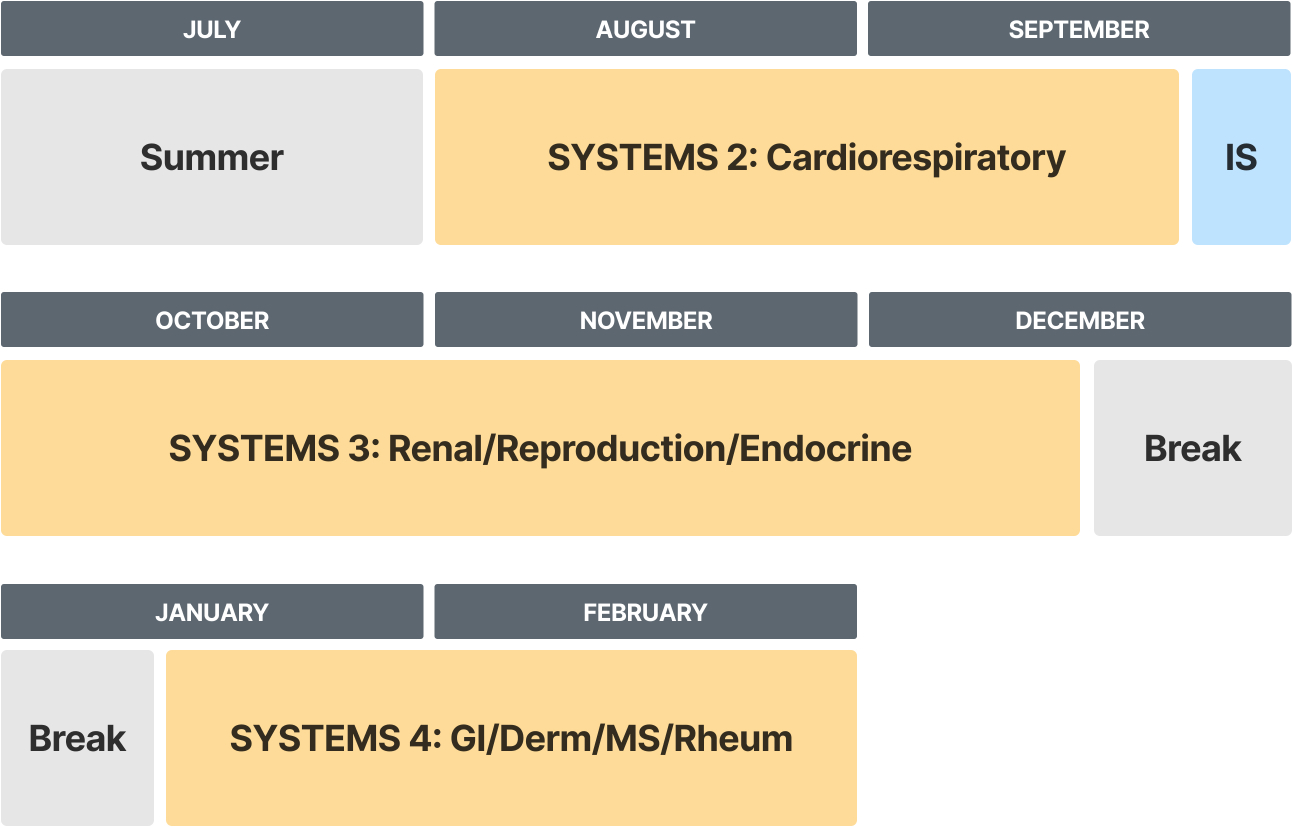
KEY- IS1-5: Health System Science Intersessions. This is a sample schedule. Individual student schedules may differ. Curriculum subject to change.
Chart Description
A sample schedule of phase 1 of year 2 of the M.D. program. It starts with summer break in July, followed by “Systems 2: Cardiology”, which runs from August through three-quarters of September. Then “IS” begins and runs until the end of September. In October, “Systems 3: Renal/Reproduction/Endocrine” begins and runs through mid-December, when break starts. Around mid-January, “Systems 4: GI/Derm/MS/Rheum” begins and runs until the end of February.
Phase Two / Core Clerkship Phase
Phase Two of the curriculum begins with a Transition to Clerkship course, a skill-building program that promotes medical student success during the Core Clerkship phase of the curriculum. You'll go on required clerkship rotations in medicine, surgery, pediatrics, obstetrics and gynecology, psychiatry, neurology, rehabilitation medicine, and family medicine. You also have built-in elective time to explore additional career options during this phase. In addition, students have a two-week “Flex” block to use for additional career exploration or to support trainee well-being.
During clinical rotations, you’ll broaden your knowledge of the manifestations of disease processes and continue to develop your skills in evidenced-based practice, critical thinking and problem solving. During this phase, students are fully engaged members of interprofessional medical teams and rotate in both inpatient and ambulatory settings.
Students take the United States Medical Licensing Examination® (USMLE) Step 2 after completing Phase Two of the M.D. Program.
Phase Two Electives
The purpose of the electives program in Phase Two of the M.D. Program is to support your career exploration process. You can use your Phase Two electives to familiarize yourself with the scope of practice in a medical specialty, typically beyond required clerkship disciplines.
Phase 2, Year 2:

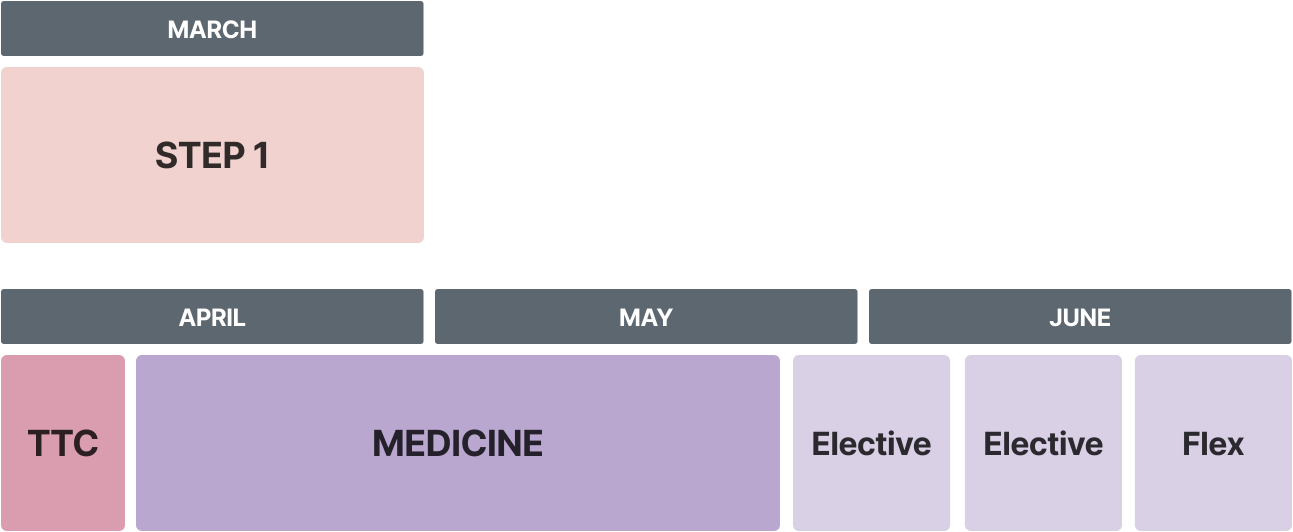
KEY- TTC: Transition to Clerkships, Flex: Variable Time For Elective or Vacation. This is a sample schedule. Individual student schedules may differ. Curriculum subject to change.
Chart Description
A sample schedule of phase 2 of year 2 of the M.D. program. “Step 1” is for the duration of March. “TTC” is for the first third of April, and then “Medicine” starts and runs until the last quarter of May. Then two electives run consecutively through the first half of June, then “Flex” until the end of June.
Phase 2, Year 3:
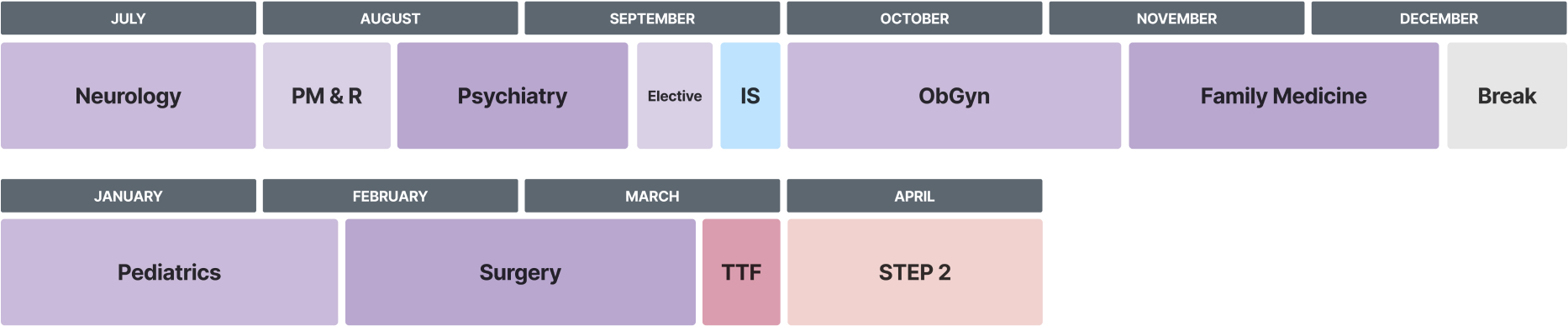
KEY: PM&R: Physical Medicine and Rehabilitation, IS1-5: Health System Science Intersessions, TTF: Transition to Fourth Year. This is a sample schedule. Individual student schedules may differ. Curriculum subject to change.
Chart Description
A sample schedule of phase 2 of year 3 of the M.D. program. “Neurology” is for the duration of July. “PM & R” is for the first half of August, and then “Psychiatry” begins and runs through the first half of September. The rest of September consists of “Elective” and then “IS”. “ObGyn” starts in October and runs through the first third of November. Then “Family Medicine” begins and runs through the first half of December. Then break through the rest of December. “Pediatrics” begins in January and continues through the beginning of February. Then “Surgery” takes place through two-thirds of March. The last third of March is “TTF”. “Step 2” runs through all of April.
Phase Three / Advanced Practice Phase
Phase Three / Advanced Practice Phase begins with a one-week transition course to prepare you for both the increasing responsibility in Phase Three of the curriculum and provide dedicated time to support you as you prepare residency applications.
Phase Three of the curriculum is organized into specialty tracks, allowing you to align your schedule with your career trajectory and maximize preparation for residency training. General requirements of this phase include a sub-internship, advanced clinical courses aligned with your specialty track, and several elective blocks to pursue areas of individual interest. Additionally, all students are enrolled in a Transition to Residency capstone course, which provides enhanced and focused skill-building opportunities individualized to the specialty in which you will be pursuing residency training.
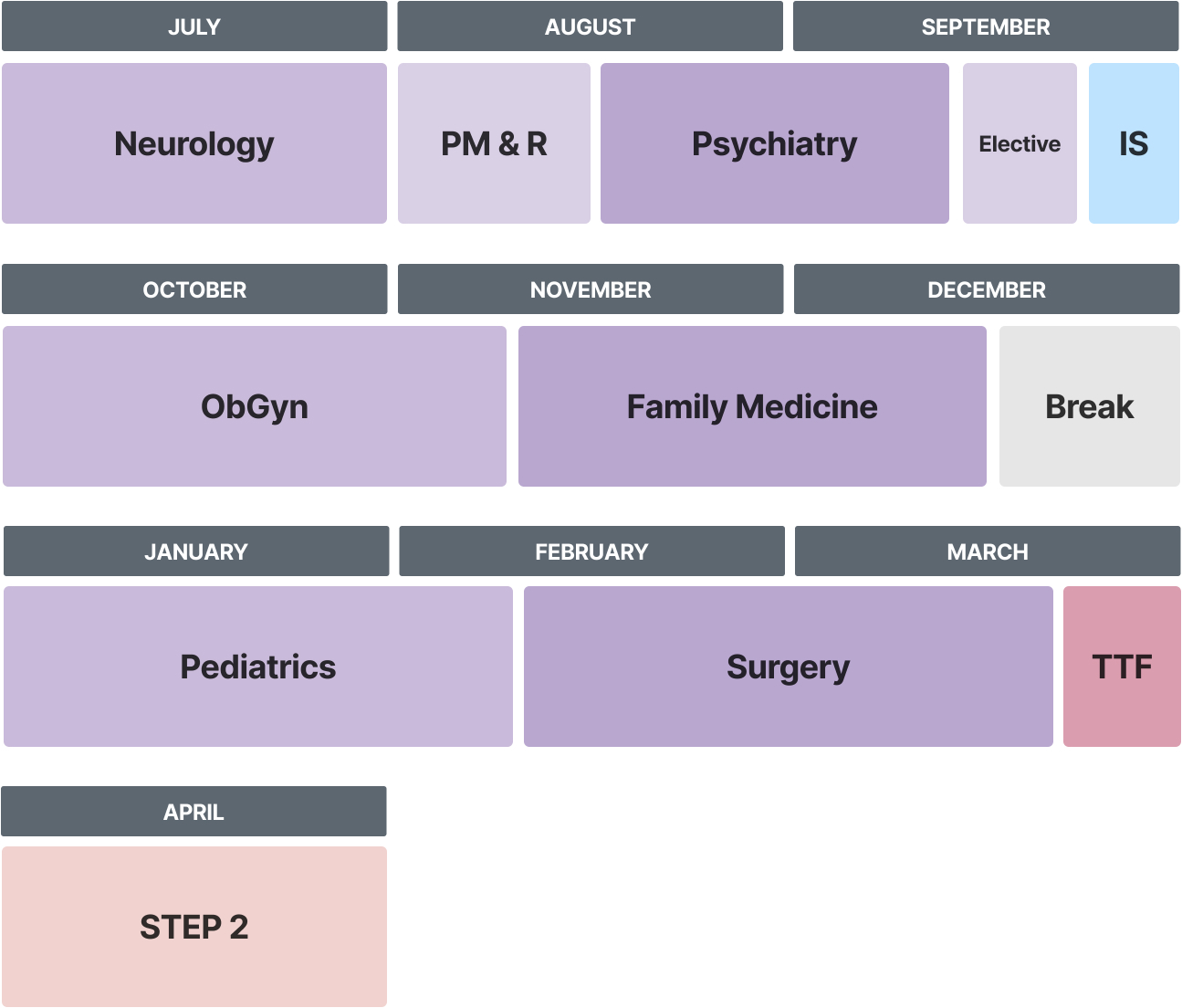
Phase 3, Year 3:

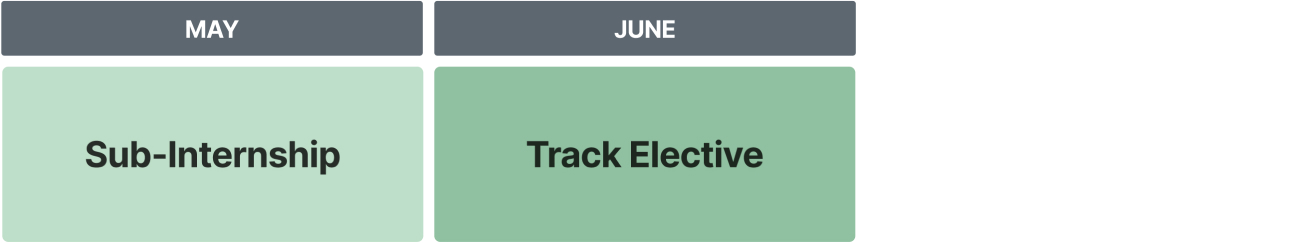
Chart Description
A sample schedule of phase 3 of year 3 of the M.D. program. “Sub-Internship” is for the duration of May, and “Track Elective” is for the duration of June.
Phase 3, Year 4:
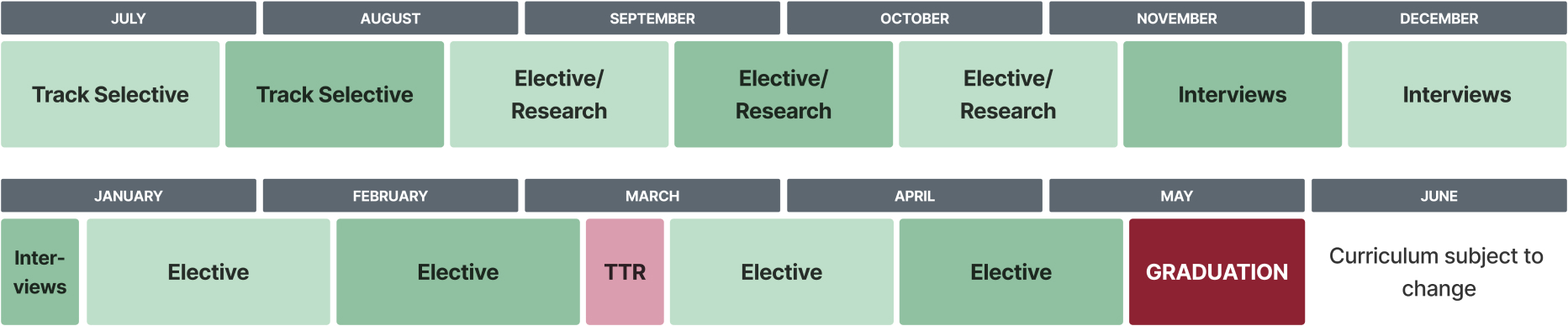
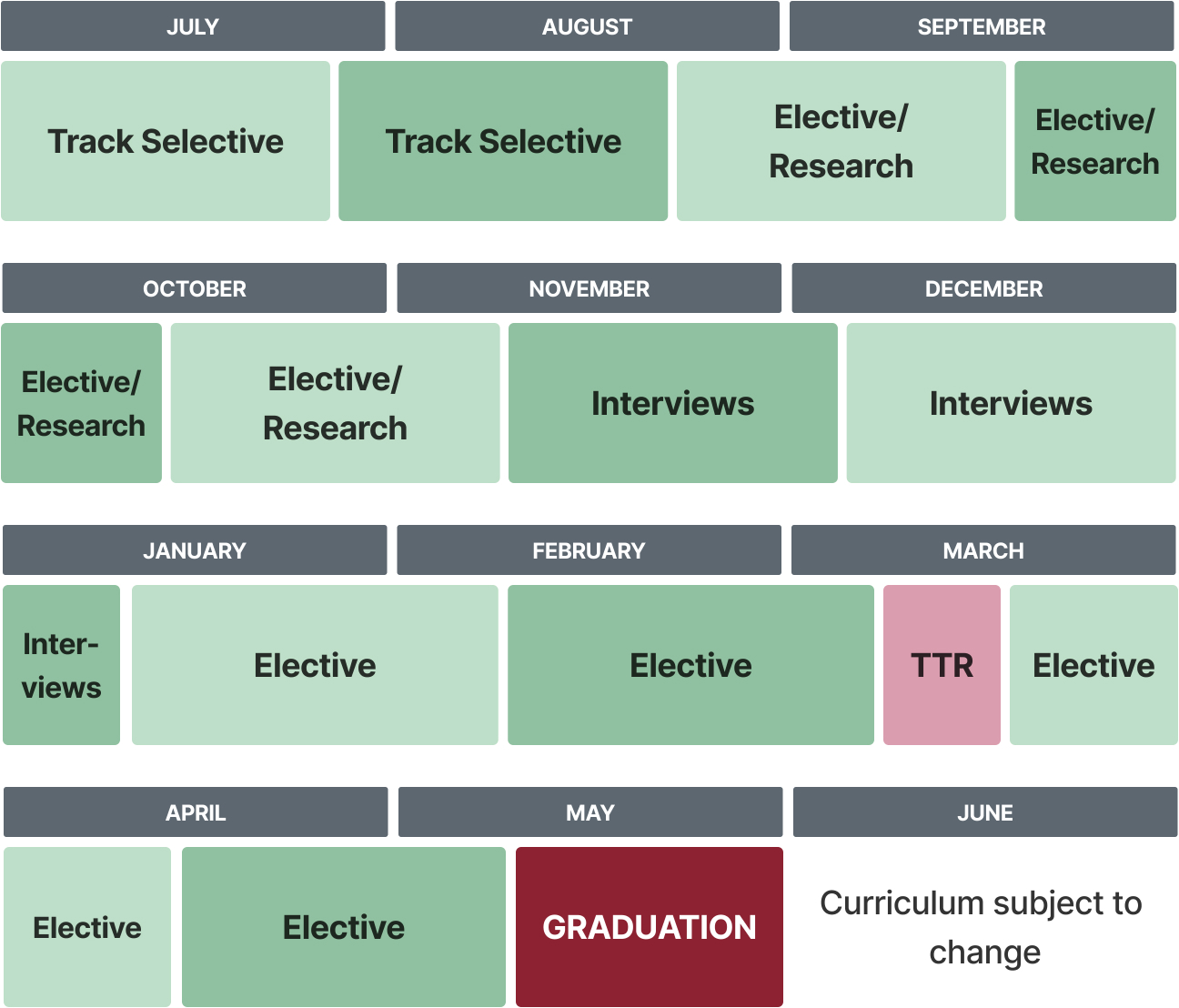
KEY- TTR: Transition to Residency. This is a sample schedule. Individual student schedules may differ. Curriculum subject to change.
Chart Description
A sample schedule of phase 3 of year 4 of the M.D. program. A “Track Selective” occurs for most of July, and then another “Track Selective” takes place through two-thirds of August. Then three “Elective/Research” classes occur consecutively from the end of August through the first part of November. Three “Interviews” phases then occur consecutively through the first part of January, then two “Elective” phases occur consecutively through the beginning of March. “TTR” runs through the middle of March, and then two “Elective” phases run consecutively through the first part of May. Then “Graduation” occurs.
Areas of Concentration
The Areas of Concentration (AOC) provides elective opportunities for medical students to differentiate themselves and pursue an area of personal interest in depth during medical school beyond the required M.D. Program curriculum. In this program, you complete additional coursework in your area of focused study and are awarded a certificate after completing a scholarly capstone project. Available areas of concentration include biomedical research, culinary medicine, health policy, medical education, biomedical ethics, global and population health, children’s environmental health and more.
Visit our Areas of Concentration page to learn more about the requirements and courses.
Office of Undergraduate Medical Education
The NYMC SOM Office of Undergraduate Medical Education (UME) is responsible for the general oversight, management and evaluation of the M.D. Program curriculum. The Office works collaboratively with all members of the New York Medical College community - faculty, students, staff and other administrators - to facilitate the delivery of an outstanding curriculum. The UME office does this by:
- Supporting the faculty and faculty committees responsible for the design and implementation of the curriculum
- Monitoring and collecting outcome data to ensure students reach program objectives and to ensure continuous quality improvement
- Promoting a learning environment that is supportive of and conducive to personal and professional development
- Facilitating the development of a comprehensive and fair system of medical student assessment that protects both medical students and Patients
- Advocating for resources necessary to achieve educational goals
Additionally, the Office supports all education committees in the SOM, including: the Education and Curriculum Committee, the Phase 1 Curriculum Subcommittee, the Phase 2 & 3 Curriculum Subcommittee, the Course/Clerkship Review Subcommittee, the Student Assessment Subcommittee and the Curricular and Thematic Integration Committee.
Contact:
Sunshine Cottage, Second floor
SOM Office of Undergraduate Medical Education
New York Medical College
40 Sunshine Cottage Road
Valhalla, NY 10595
(914) 594-3900
(914) 594-3960 (fax)


